Enamel hypoplasia weakens your teeth by causing thin or missing enamel, leaving them vulnerable to decay, sensitivity, and damage. If you or your child has this condition, early intervention is key to preventing serious dental problems. Treatment options range from fluoride treatments and sealants to dental bonding or crowns, depending on severity. Maintaining excellent oral hygiene and avoiding sugary or acidic foods can help protect your teeth. Consult a dentist to create a personalized plan—ignoring enamel hypoplasia can lead to painful complications and costly repairs.
Unraveling the Causes of Enamel Hypoplasia
Enamel hypoplasia stems from disruptions during tooth development, whether from external triggers or inherent biological factors. Identifying the root cause helps tailor treatment and preventive strategies, whether addressing environmental exposures or managing genetic predispositions.
Environmental and Infectious Agents
Prenatal infections like rubella or syphilis can impair enamel formation in developing fetuses, while childhood illnesses such as measles or prolonged high fevers disrupt ameloblast function. Environmental toxins—excessive fluoride, lead, or tetracycline antibiotics—also create structural defects. Regions with fluorosis prevalence above 1.5 ppm fluoride in water show a 23% higher incidence of enamel hypoplasia.
Try Our Dental Calculators
Genetic and Autoimmune Predispositions
Mutations in genes like AMELX, ENAM, or MMP20 directly affect enamel matrix proteins, leading to conditions like amelogenesis imperfecta. Autoimmune disorders such as celiac disease may trigger enamel defects due to nutrient malabsorption or immune-mediated damage to developing teeth.
Studies reveal that 70% of celiac patients exhibit enamel hypoplasia, often symmetrically in permanent teeth. Genetic testing can pinpoint variants like FAM83H mutations, which cause severe hypomineralization. Early identification allows for interventions like sealants or dietary adjustments to mitigate damage before permanent teeth erupt.
Recognizing the Symptoms and Complications
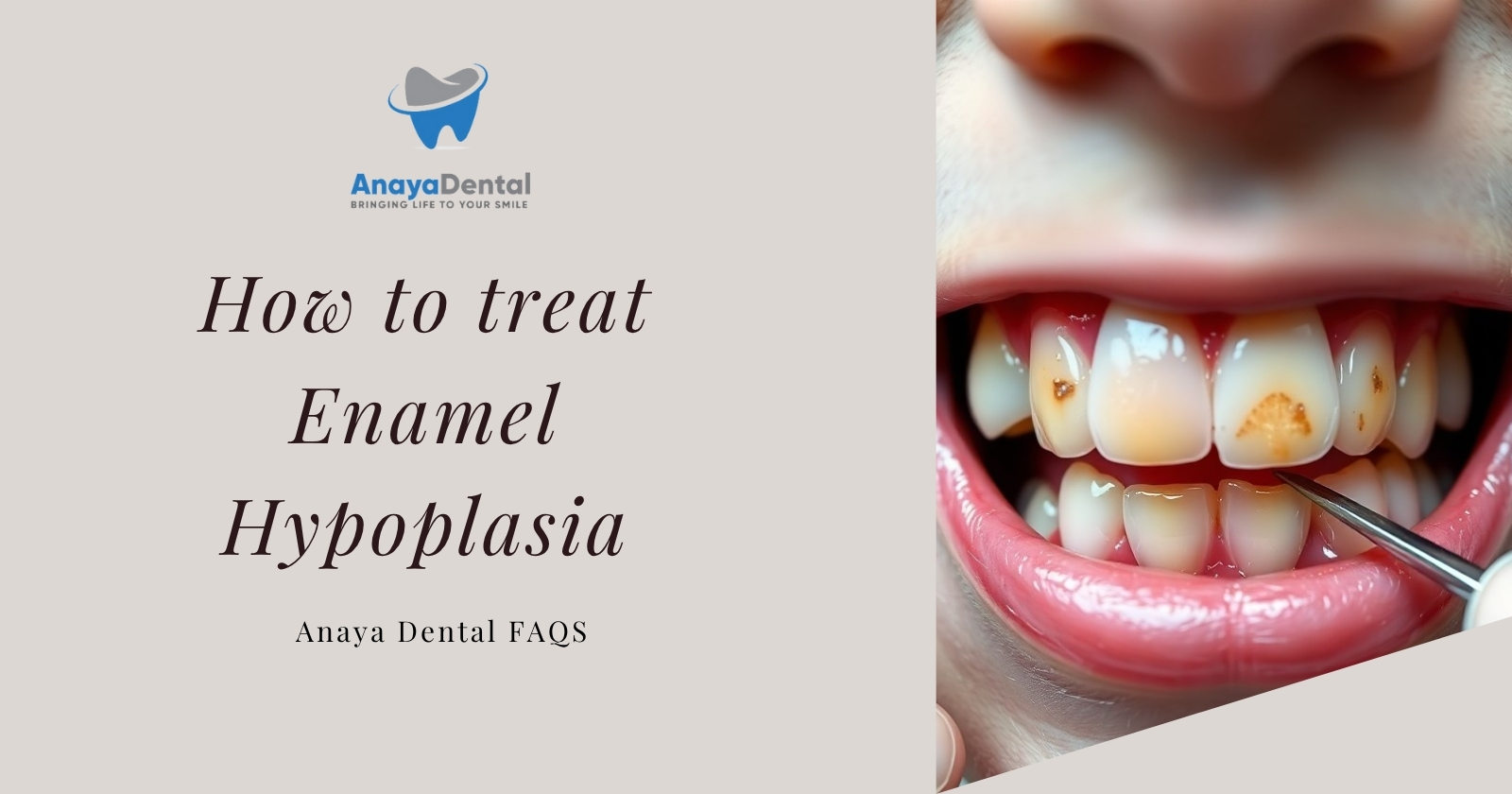
Spotting enamel hypoplasia early can prevent irreversible damage to your teeth. The condition often presents with visible enamel irregularities, heightened sensitivity, or rapid tooth decay—signs that demand prompt attention to avoid escalating oral health issues.
Identifying Common Signs
White or brown spots, pits, or grooves on tooth surfaces are hallmark indicators of enamel hypoplasia. You might notice increased tooth sensitivity to hot, cold, or sweet stimuli, or teeth that appear smaller or misshapen. In severe cases, enamel may chip easily, exposing the vulnerable dentin underneath.
Understanding Potential Complications of Neglect
Ignoring enamel hypoplasia can lead to aggressive cavities, abscesses, or premature tooth loss. A 2019 study in the *Journal of Dental Research* found that untreated hypoplastic teeth are 3x more likely to require root canals or extractions due to structural weakness and bacterial invasion.
Without intervention, complications extend beyond aesthetics. Exposed dentin accelerates wear, leading to chronic pain and bite misalignment. Children with severe hypoplasia may face speech delays or nutritional deficits from avoiding hard or cold foods. Early restorative treatments, like sealants or crowns, can mitigate these risks.
Diagnostic Pathways: From Assessment to Tests
Diagnosing enamel hypoplasia involves a combination of clinical assessments and specialized tests to confirm the condition and rule out similar dental disorders. Your dentist will evaluate visible enamel defects, review your medical history, and may use imaging or other diagnostic tools to pinpoint the extent of enamel loss. Early and accurate diagnosis is key to preventing complications like severe tooth decay or structural damage.
Clinical Assessments by Dental Professionals
During a clinical exam, your dentist will inspect your teeth for pits, grooves, or discoloration—common signs of enamel hypoplasia. They’ll assess sensitivity to temperature or pressure and review factors like childhood illnesses, nutritional deficiencies, or genetic conditions that could contribute to enamel defects. In one study, 60% of cases were identified through visual examination alone, highlighting its importance in initial screening.
Utilizing Diagnostic Tools for Accurate Identification
For borderline or complex cases, tools like dental X-rays or transillumination (light-based imaging) help measure enamel thickness and detect subsurface defects. Advanced methods such as optical coherence tomography (OCT) can reveal microstructural enamel abnormalities undetectable to the naked eye.
Bitewing X-rays are particularly useful for identifying enamel loss between teeth, while intraoral cameras document progression over time. In pediatric cases, dentists may use laser fluorescence devices to quantify mineral loss, with studies showing a 92% accuracy rate in distinguishing hypoplasia from similar conditions like fluorosis. Combining these tools reduces misdiagnosis risks and tailors treatment plans to your specific enamel needs.
Effective Treatment Strategies for Enamel Hypoplasia
Managing enamel hypoplasia requires a tailored approach to protect weakened enamel and prevent complications like cavities or tooth sensitivity. Dental bonding, sealants, or crowns may be recommended to restore structural integrity, while fluoride varnishes can strengthen remaining enamel. For severe cases, pediatric dentists often use stainless steel crowns on primary teeth to preserve function until permanent teeth emerge. Early intervention reduces the risk of long-term damage, with studies showing a 60% decrease in cavity formation when treated before age 6.
Medical Interventions for Symptom Management
Prescription-strength fluoride toothpaste (5,000 ppm) or silver diamine fluoride may be applied to halt decay in hypoplastic teeth. For pain from sensitivity, desensitizing agents like potassium nitrate or glass ionomer cements provide relief. Antibiotics are reserved for rare infections stemming from enamel defects, while calcium phosphate remineralization pastes (e.g., MI Paste) help rebuild surface minerals.
Embracing Non-Pharmacological Approaches
Dietary adjustments—like limiting acidic foods (pH <5.5) and increasing calcium-rich dairy or leafy greens—support enamel health. Chewing xylitol gum stimulates saliva production, which naturally remineralizes teeth, while soft-bristled toothbrushes prevent further enamel abrasion.
Behavioral modifications also play a role: nighttime teeth grinding (bruxism) can be mitigated with custom mouthguards, and drinking through a straw minimizes acid contact with teeth. A 2022 study found that patients combining these strategies saw a 40% reduction in enamel erosion progression over six months compared to those relying solely on medical treatments.
Preventive Measures to Safeguard Enamel Health
Protecting your enamel from hypoplasia starts with proactive habits that minimize risk factors. Fluoride treatments, sealants, and regular dental checkups can strengthen vulnerable enamel, while avoiding excessive sugar or acidic foods reduces erosion. For children, monitoring developmental milestones and addressing nutritional deficiencies early can prevent enamel defects.
Nutritional Strategies for Stronger Enamel
A diet rich in calcium, phosphorus, and vitamin D supports enamel mineralization—think dairy, leafy greens, and fortified foods. Studies show children with adequate vitamin D intake have a 30% lower risk of enamel defects. Limit citrus and soda, which leach minerals from teeth.
The Role of Oral Hygiene in Prevention
Brushing twice daily with soft-bristled brushes and fluoride toothpaste removes plaque without damaging thin enamel. Flossing prevents interdental decay, a common issue in hypoplastic teeth. Research indicates electric toothbrushes reduce enamel wear by 18% compared to manual brushing.
For those with enamel hypoplasia, avoid abrasive whitening toothpastes—they accelerate enamel loss. Instead, opt for remineralizing gels containing calcium phosphate. A 2022 study found patients using prescription-strength fluoride gels saw a 40% reduction in cavity formation. Pair this with biannual professional cleanings to monitor enamel integrity.
Final Words
So, treating enamel hypoplasia involves protecting your teeth from further damage while addressing sensitivity and decay risks. You can use fluoride treatments to strengthen enamel, dental sealants to shield vulnerable areas, and bonding or crowns for severe cases. Maintain a consistent oral hygiene routine with a soft-bristled brush and avoid acidic or sugary foods. Regular dental check-ups will help monitor your condition and adjust treatments as needed. By taking these steps, you can manage enamel hypoplasia effectively and preserve your oral health.
FAQ
Q: What are the most effective treatments for enamel hypoplasia?
A: Treatment options for enamel hypoplasia depend on the severity of the condition. Common approaches include dental bonding, sealants, or crowns to protect weakened enamel. Fluoride treatments may help strengthen remaining enamel, while desensitizing agents can reduce tooth sensitivity. In severe cases, veneers or full-coverage restorations may be recommended to improve both function and appearance.
Q: Can enamel hypoplasia be reversed or repaired naturally?
A: Enamel hypoplasia cannot be reversed naturally because enamel does not regenerate once formed. However, early intervention can prevent further damage. Maintaining excellent oral hygiene, using remineralizing toothpaste, and following a nutrient-rich diet (high in calcium, phosphorus, and vitamin D) may help support existing enamel. Regular dental check-ups are necessary to monitor the condition.
Q: How does enamel hypoplasia differ from enamel erosion, and does this affect treatment?
A: Enamel hypoplasia is a developmental defect where enamel is thin or missing from the start, while erosion occurs when acid wears down healthy enamel over time. Treatment differs because hypoplasia often requires structural reinforcement (e.g., bonding or crowns) to compensate for missing enamel, whereas erosion focuses on halting acid exposure and protecting remaining enamel. Both conditions benefit from fluoride therapy and dietary adjustments.