Fluoride in Toothpaste: Weighing the Benefits and Risks
For decades, fluoride has been celebrated as a dental care essential, known for its ability to strengthen enamel and reduce cavities. However, recent research and public health debates have raised questions about its safety, particularly regarding long-term exposure and potential risks for certain populations. This comprehensive guide examines the science behind fluoride, helping you make informed decisions about your oral health care routine.
How Fluoride Works: The Science Behind Cavity Prevention
Fluoride is a naturally occurring mineral found in soil, water, and certain foods. When applied topically through toothpaste, fluoride forms fluorapatite, a compound that’s more resistant to acid erosion than the natural hydroxyapatite in our teeth. This chemical reaction is the foundation of fluoride’s cavity-fighting properties.
At the microscopic level, fluoride works through several mechanisms:
Try Our Dental Calculators
- Remineralization: Fluoride accelerates the repair of weakened enamel by attracting calcium and phosphate ions to damaged areas
- Acid resistance: The fluorapatite crystals formed are less soluble in acid compared to natural tooth minerals
- Antimicrobial action: Fluoride disrupts bacterial metabolism, inhibiting the production of acid that causes tooth decay
The widespread adoption of fluoridated toothpaste in the mid-20th century coincided with significant declines in global dental caries rates, with some studies showing a 20-40% reduction in cavities. However, there’s a fine line between therapeutic benefit and potential toxicity. According to the U.S. National Institutes of Health, the recommended daily fluoride intake is 0.05 mg/kg body weight for children and 3–4 mg for adults.
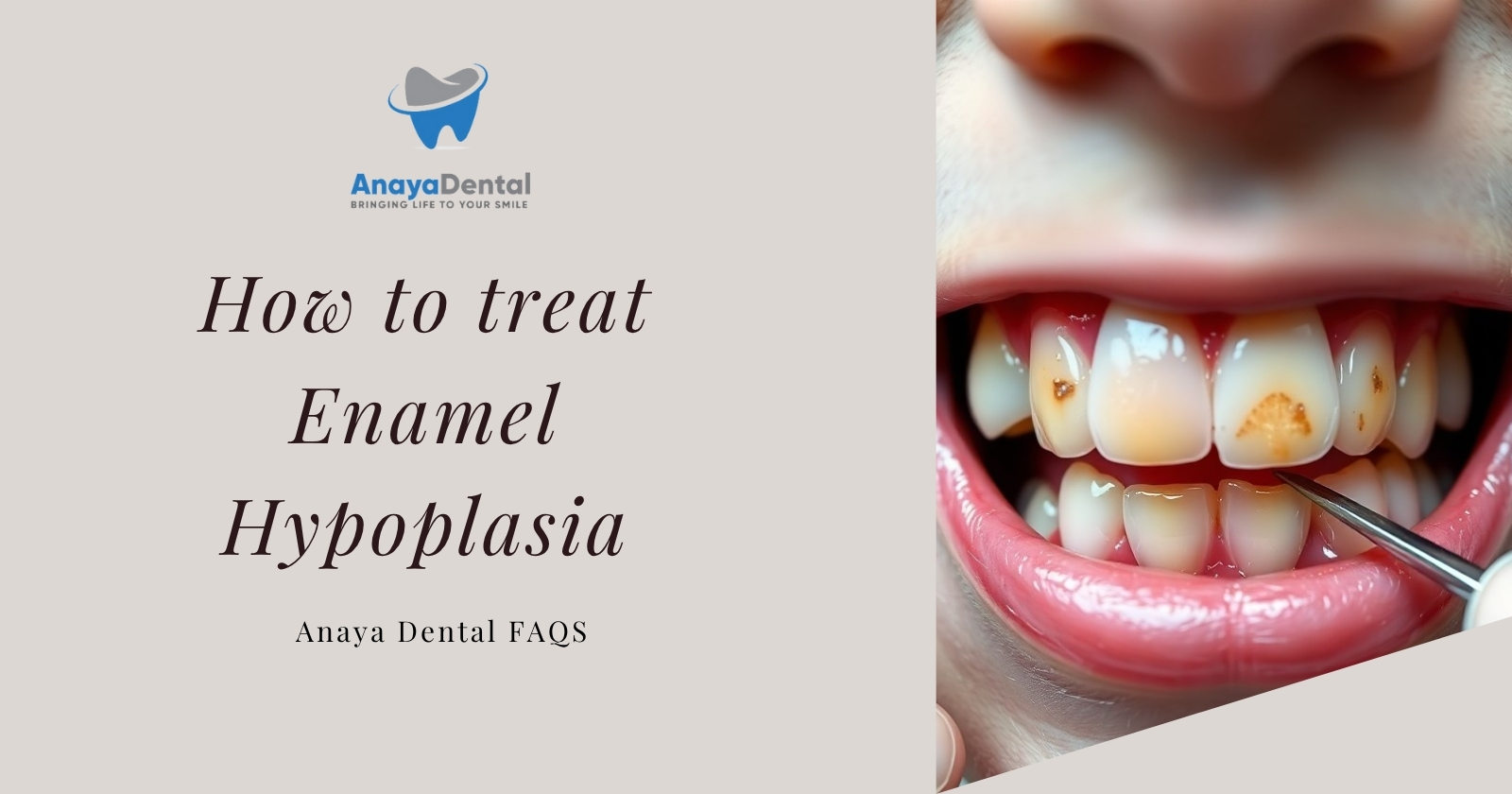
Dental Fluorosis: Understanding the Visible Effects
Dental fluorosis, characterized by white streaks or brown staining on teeth, occurs from excessive fluoride intake during enamel formation (ages 0–8). A 2019 study found that 31.3% of dentists and 16.5% of non-dental physicians expressed concern about fluorosis risk in children using fluoride toothpaste.
Fluorosis severity ranges from:
- Very mild: Barely noticeable white flecks covering less than 25% of tooth surfaces
- Mild: White opaque areas affecting less than 50% of the surface
- Moderate: All tooth surfaces affected, with possible brown staining
- Severe: All enamel surfaces affected with discrete pitting and brown staining
Epidemiological data from the NHANES survey (1999–2004) showed that 20.8% of Americans aged 6–49 exhibited some form of fluorosis, with severe cases linked to early childhood toothpaste ingestion.
The CDC reports that 40% of children aged 3–6 use more toothpaste than recommended, which increases the risk of fluorosis. A pea-sized amount (0.25 g) contains approximately 0.25 mg fluoride, but many parents apply 5–7 times this dose. This is particularly problematic because children under 6 swallow 30–50% of toothpaste during brushing, compared to just 10% in adults.
Beyond Aesthetics: Skeletal and Systemic Concerns
Chronic overexposure to fluoride can accumulate in bones, leading to skeletal fluorosis—a condition marked by joint stiffness, osteoporosis, and fractures. While rare in regions with optimally fluoridated water (0.7 ppm), endemic cases persist in areas like India and China where natural fluoride levels exceed 4 ppm.
The progression of skeletal fluorosis typically occurs in stages:
- Preclinical phase: Asymptomatic bone changes detectable only by radiographs
- Early clinical phase: Joint pain, stiffness, and osteosclerosis (increased bone density)
- Crippling phase: Calcification of ligaments, limited joint mobility, and potential deformity
Animal studies indicate that fluoride alters osteoblast activity and collagen synthesis, potentially increasing bone brittleness despite higher mineral density. This apparent paradox explains why fluorosis can sometimes lead to increased fracture risk despite denser bone appearance on scans.
Neurodevelopmental Concerns: The Emerging Research
Recent studies have sparked debate about fluoride’s potential neurotoxicity. A 2024 lawsuit in San Francisco highlighted evidence linking maternal fluoride exposure to lower IQ scores in offspring. Meta-analyses suggest that each 1 mg/L increase in urinary fluoride correlates with a 3.7-point IQ reduction, though critics argue these findings derive from high-dose exposures that may not be relevant to toothpaste use.
Experimental models propose several mechanisms for fluoride’s potential neurotoxicity:
- Oxidative stress: Fluoride may generate free radicals that damage neuronal cell membranes
- Thyroid disruption: Altered thyroid hormone levels could affect brain development
- Blood-brain barrier interference: Fluoride might compromise this protective barrier
- Neurotransmitter modulation: Studies suggest changes in acetylcholine and dopamine systems
However, the National Toxicology Program’s systematic review (2025) concluded evidence remains “inconsistent” for doses under 1.5 ppm, the level typically found in fluoridated water. Most experts agree that the risk from properly used fluoride toothpaste, especially when not swallowed, is minimal compared to systemic exposures.
Endocrine Disruption: Potential Impact on Hormonal Health
Fluoride’s structural similarity to iodide enables it to potentially interfere with thyroid hormone synthesis. A 2023 review linked excessive fluoride intake to hypothyroidism, particularly in iodine-deficient populations. In animal studies, 5 ppm fluoride reduced T4 levels by 30%.
Human data are less conclusive, though ecological studies have noted higher hypothyroidism rates in fluoridated communities (e.g., 6.5% vs. 4.3% in non-fluoridated areas). The potential mechanisms include:
- Competition with iodine uptake in the thyroid gland
- Inhibition of thyroid peroxidase, a key enzyme in thyroid hormone production
- Disruption of deiodinase enzymes that convert T4 to the active T3 form
Those with pre-existing thyroid conditions may want to discuss fluoride exposure with their healthcare providers, as individual susceptibility varies significantly.
Special Considerations for Vulnerable Groups
Children Under 6
Children under 6 are particularly susceptible to fluoride overexposure due to their developing dentition and swallowing reflexes. The American Academy of Pediatric Dentistry recommends:
- For children under 3: Use only a rice-grain sized smear of toothpaste (approximately 0.1 g)
- For children 3-6: Use a pea-sized amount of toothpaste (approximately 0.25 g)
- Supervision during brushing to ensure proper spitting and rinsing
- Storing toothpaste out of reach to prevent unsupervised use and potential ingestion
Pregnant and Nursing Women
Recent research suggests that maternal fluoride exposure during pregnancy may affect fetal development. While definitive conclusions remain elusive, pregnant women might consider:
- Consulting with healthcare providers about fluoride intake from all sources
- Using appropriate amounts of fluoride toothpaste while minimizing swallowing
- Being aware of water fluoride levels in their community
Individuals with Specific Health Conditions
People with certain conditions may need to exercise additional caution:
- Kidney disease: Reduced ability to excrete fluoride may lead to higher body burden
- Thyroid disorders: Potential interaction with thyroid function
- Fluoride sensitivity: Some individuals report adverse reactions to fluoride products
Additionally, individuals living in areas with naturally high fluoride water levels (>1.5 ppm) should consider avoiding fluoridated toothpaste to prevent cumulative exposure.
Fluoride-Free Alternatives: Evidence-Based Options
For those concerned about fluoride, several evidence-based alternatives exist:
Calcium Hydroxyapatite (CaHA)
This biomimetic compound has emerged as a leading fluoride alternative. Clinical trials show CaHA toothpaste reduces caries incidence by 32% compared to placebo, matching fluoride’s efficacy without toxicity risks. Benefits include:
- Biocompatibility: CaHA is identical to the mineral naturally present in teeth
- Remineralization capacity: Provides calcium and phosphate ions directly to tooth surfaces
- Whitening properties: Can help reduce staining without abrasiveness
- No toxicity concerns: Safe if accidentally swallowed
A 2023 clinical trial demonstrated that nano-hydroxyapatite toothpaste was non-inferior to fluoride for preventing early caries lesions, particularly encouraging for high-risk populations seeking alternatives.
Xylitol-Based Products
This natural sweetener offers multiple oral health benefits:
- Reduces Streptococcus mutans adhesion to tooth surfaces
- Disrupts bacterial metabolism, preventing acid production
- Stimulates saliva flow, enhancing natural remineralization
- Neutral pH helps maintain oral acid-base balance
Research suggests optimal benefits occur at 6-10g daily exposure, achievable through combined use of xylitol toothpaste, mints, and gum.
Enzyme-Based Formulations
These innovative products use enzymes like glucoamylase and lactoperoxidase to disrupt plaque biofilm formation:
- Break down bacterial food sources before they can cause damage
- Enhance natural salivary enzyme activity
- Provide continued protection between brushing sessions
- Work synergistically with other natural ingredients
Making Informed Choices: Practical Guidelines
The decision to use fluoride toothpaste involves weighing its proven anti-caries benefits against potential risks, particularly for children and high-risk groups. While dental fluorosis remains the most common adverse effect, emerging concerns about neurodevelopmental and endocrine impacts warrant further study.
Assessing Your Personal Risk Profile
Consider these factors when making decisions about fluoride use:
- Your cavity history: Those with recurrent decay may benefit more from fluoride
- Local water fluoridation status: Check your municipal water reports for fluoride levels
- Age and developmental stage: Children have different considerations than adults
- Existing health conditions: Some medical conditions may alter risk-benefit calculations
- Dietary factors: High sugar consumption increases decay risk and may influence fluoride needs
Practical Tips for Safe Fluoride Use
If you choose to use fluoride toothpaste:
- Follow age-appropriate dosing guidelines for toothpaste application
- Supervise young children during brushing to prevent excessive swallowing
- Spit thoroughly after brushing and avoid rinsing immediately to maximize topical benefits
- Wait 30 minutes after brushing before eating or drinking
- Consider fluoride-free options for children who can’t reliably spit
- Store fluoride products securely away from young children
- Consider your total fluoride exposure from multiple sources (water, food, dental products)
Optimizing Oral Health Beyond Toothpaste Choice
Regardless of your toothpaste preferences:
- Brush thoroughly twice daily for two minutes each time
- Use proper brushing technique with a soft-bristled brush
- Floss daily to remove interdental plaque
- Limit sugary foods and drinks, especially between meals
- Stay hydrated to maintain adequate saliva flow
- Visit dental professionals regularly for check-ups and professional cleaning
- Consider additional preventive measures like dental sealants for high-risk individuals
The Future of Dental Care: Emerging Technologies
The dental care landscape continues to evolve, with several promising developments:
- Bioactive glass technology: Releases calcium and phosphate ions while forming a protective layer on teeth
- Probiotics for oral health: Targeted beneficial bacteria to counter cavity-causing species
- Smart toothbrushes with monitoring capabilities: Provide feedback on brushing effectiveness
- Targeted antimicrobial peptides: Selectively eliminate harmful bacteria while preserving beneficial oral flora
Conclusion: Balancing Tradition and Innovation
Whether you choose fluoride or fluoride-free options, consistent brushing, flossing, and regular dental check-ups remain the cornerstones of good oral health. The growing body of research on both traditional fluoride and alternative compounds offers more personalized choices for different needs and preferences.
Work with dental professionals to develop an oral care regimen that addresses your specific risk factors, concerns, and health goals. By staying informed about emerging research and maintaining open communication with healthcare providers, you can make choices that support both your dental health and overall wellbeing.