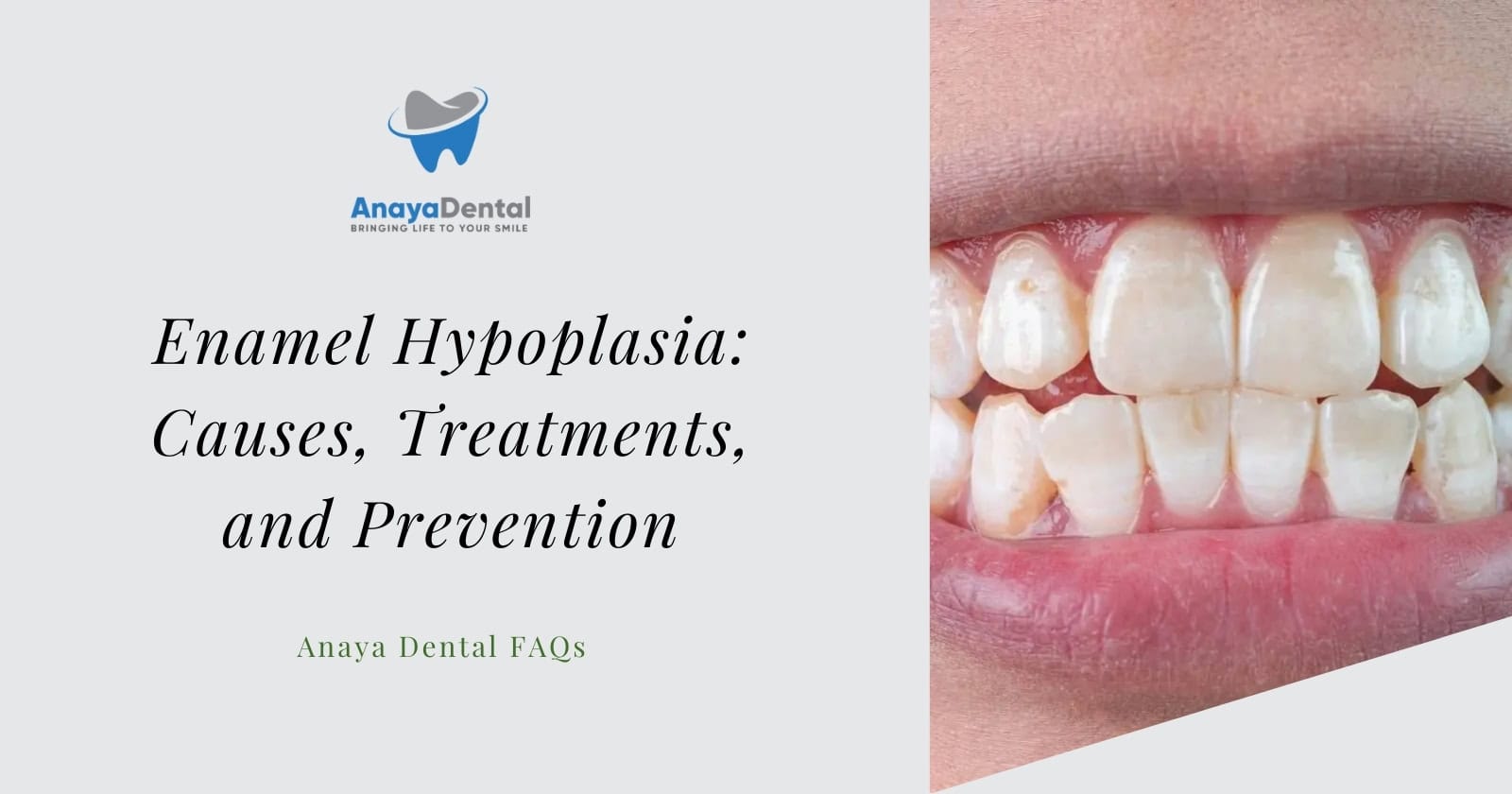
Have you ever noticed unusual white spots, lines, or pits on your teeth? These might be signs of enamel hypoplasia, a dental condition that affects the outer protective layer of your teeth. Unlike typical tooth stains that develop over time, enamel hypoplasia occurs during tooth development, resulting in teeth that emerge with visible defects already present.
Understanding Enamel Hypoplasia and Its Impact on Your Dental Health
Enamel hypoplasia occurs when there’s a disruption in the process of enamel formation during tooth development. Your tooth enamel forms through a complex biological process called amelogenesis, where specialized cells called ameloblasts secrete enamel proteins. When this process is interrupted, it leads to insufficient enamel quantity in affected areas.
Unlike other dental conditions that develop after teeth erupt, enamel hypoplasia is a developmental defect that happens before your teeth even break through the gums. The result is teeth that emerge with noticeable structural changes, often appearing as well-defined horizontal lines, pits, or grooves across multiple teeth at similar levels.
Try Our Dental Calculators
According to the American Academy of Pediatric Dentistry, enamel hypoplasia affects both primary (baby) and permanent teeth, with varying degrees of severity. The condition not only creates aesthetic concerns but can also lead to increased risk of tooth decay and sensitivity due to the compromised enamel structure.
Types of Enamel Hypoplasia You Might Experience
Hereditary Enamel Hypoplasia
This type is caused by genetic factors and often affects your entire dentition in both primary and permanent teeth. If you have hereditary enamel hypoplasia, you might notice that all your teeth display similar patterns of defects, reflecting the genetic influence on enamel development.
Hereditary enamel hypoplasia is frequently associated with conditions like:
- Amelogenesis imperfecta
- Dentinogenesis imperfecta
- Ectodermal dysplasia
These genetic conditions affect the quality and quantity of enamel in predictable patterns across your entire dentition.
Environmental Enamel Hypoplasia
Unlike the hereditary type, environmental enamel hypoplasia affects only those teeth that were developing during a specific disturbance period. This means you might notice defects on certain teeth while others appear completely normal.
Environmental factors that can lead to this type include:
- Nutritional deficiencies during childhood
- Severe illnesses or infections
- Physical trauma to developing teeth
- Premature birth complications
- Exposure to certain medications or chemicals
The pattern of affected teeth often provides clues about when the disruption occurred, as different teeth develop at different stages of childhood.
The Science Behind the Formation of Your Tooth Enamel
To truly understand enamel hypoplasia, you need to know how your tooth enamel normally forms. Enamel development follows a precise timeline:
- Secretory Phase: Ameloblasts secrete enamel matrix proteins that establish the framework for enamel.
- Maturation Phase: The matrix undergoes mineralization as calcium and phosphate crystals are deposited.
- Final Hardening: Water is removed and crystals grow, creating the hardest substance in your body.
Your permanent central incisors begin calcification at 3-4 months of age, with lateral incisors following at 10-12 months. Both complete enamel formation by ages 4-5 years, making this early childhood period especially vulnerable to factors that can affect enamel quality.
When disruptions occur during the secretory phase, you’ll typically develop hypoplasia (reduced enamel quantity). Problems during the maturation phase instead lead to hypomineralization (poor enamel quality).
Common Causes of Enamel Hypoplasia in Your Teeth
Genetic Factors That Influence Enamel Development
If you have a family history of dental enamel defects, you may be more susceptible to hereditary forms of enamel hypoplasia. Genetic mutations affecting the genes responsible for enamel formation (AMELX, ENAM, MMP20, and KLK4) can result in various types of amelogenesis imperfecta, presenting with thin, pitted, or malformed enamel.
The inheritance pattern varies depending on the specific genetic condition, with some forms being X-linked (more common in males) and others showing autosomal dominant or recessive patterns.
Nutritional Deficiencies During Key Developmental Periods
Your nutritional status during tooth development plays a crucial role in enamel formation. Deficiencies in key nutrients can significantly impact enamel quality:
- Vitamin A deficiency disrupts ameloblast function and epithelial differentiation.
- Vitamin D insufficiency reduces calcium absorption, compromising mineral availability for enamel formation.
- Calcium and phosphorus deficiencies directly affect the mineralization process.
- Protein malnutrition during early childhood can lead to defective enamel matrix production.
These nutritional impacts are particularly concerning in areas with food insecurity, where children may experience prolonged periods of inadequate nutrition during critical developmental windows.
The Impact of Illnesses and Medications on Enamel Formation
Certain childhood illnesses can significantly affect enamel development, especially when they occur during critical periods of tooth formation:
- High fevers from infections can disrupt ameloblast function.
- Respiratory illnesses may affect oxygen supply to developing tissues.
- Gastrointestinal disorders can reduce nutrient absorption necessary for proper enamel formation.
- Congenital conditions like celiac disease may interfere with nutrient utilization.
Additionally, certain medications taken during childhood can affect enamel development:
- Tetracycline antibiotics (when given before age 8)
- Some anticonvulsants
- Chemotherapy agents
- High doses of fluoride supplements
Birth-Related Factors That May Contribute to Enamel Defects
If you were born prematurely or experienced birth complications, you might have an increased risk of enamel hypoplasia. Factors that contribute to this include:
- Premature birth (especially before 32 weeks gestation)
- Very low birth weight (less than 1500g)
- Birth-related oxygen deprivation
- Neonatal jaundice requiring intensive treatment
- Intubation and mechanical ventilation (which can affect the development of primary teeth)
These birth-related factors can disrupt the normal progression of enamel formation, leading to visible defects once teeth erupt.
Recognizing the Signs and Symptoms of Enamel Hypoplasia
Visual Characteristics That Distinguish Enamel Hypoplasia
When examining your teeth, you might notice these distinctive features of enamel hypoplasia:
- Well-defined horizontal lines or grooves across multiple teeth
- Pits or depressions in the enamel surface
- Areas of thin or missing enamel exposing the yellowish dentin beneath
- White, yellow, or brownish patches with clear boundaries
- Consistent positioning of defects across several teeth, creating a “chronological” pattern
Unlike white spots from early decay (which have fuzzy boundaries), hypoplastic defects have distinct margins and often show actual structural changes in the enamel.
Associated Symptoms You Shouldn’t Ignore
Beyond the visual appearance, enamel hypoplasia often comes with other symptoms:
- Increased tooth sensitivity to temperature, sweetness, or acidity
- Higher susceptibility to dental caries in affected areas
- Rough texture when you run your tongue over affected areas
- Potential speech difficulties if front teeth are severely affected
- Dental pain when defects are deep enough to approach the dentin
Early recognition of these symptoms allows for prompt intervention before more serious complications develop.
How Dental Professionals Diagnose Enamel Hypoplasia
Your dentist will use several approaches to diagnose enamel hypoplasia:
- Visual examination in good lighting, often using magnification
- Tactile exploration with a dental probe to assess surface characteristics
- Review of your medical and developmental history
- Radiographic (X-ray) assessment to evaluate enamel thickness
- In some cases, specialized techniques like transillumination to better visualize the extent of defects
When diagnosing this condition, dental professionals look not only at the appearance of defects but also their distribution pattern, which helps identify whether the cause was a systemic issue affecting multiple teeth or a localized trauma affecting just one or two teeth.
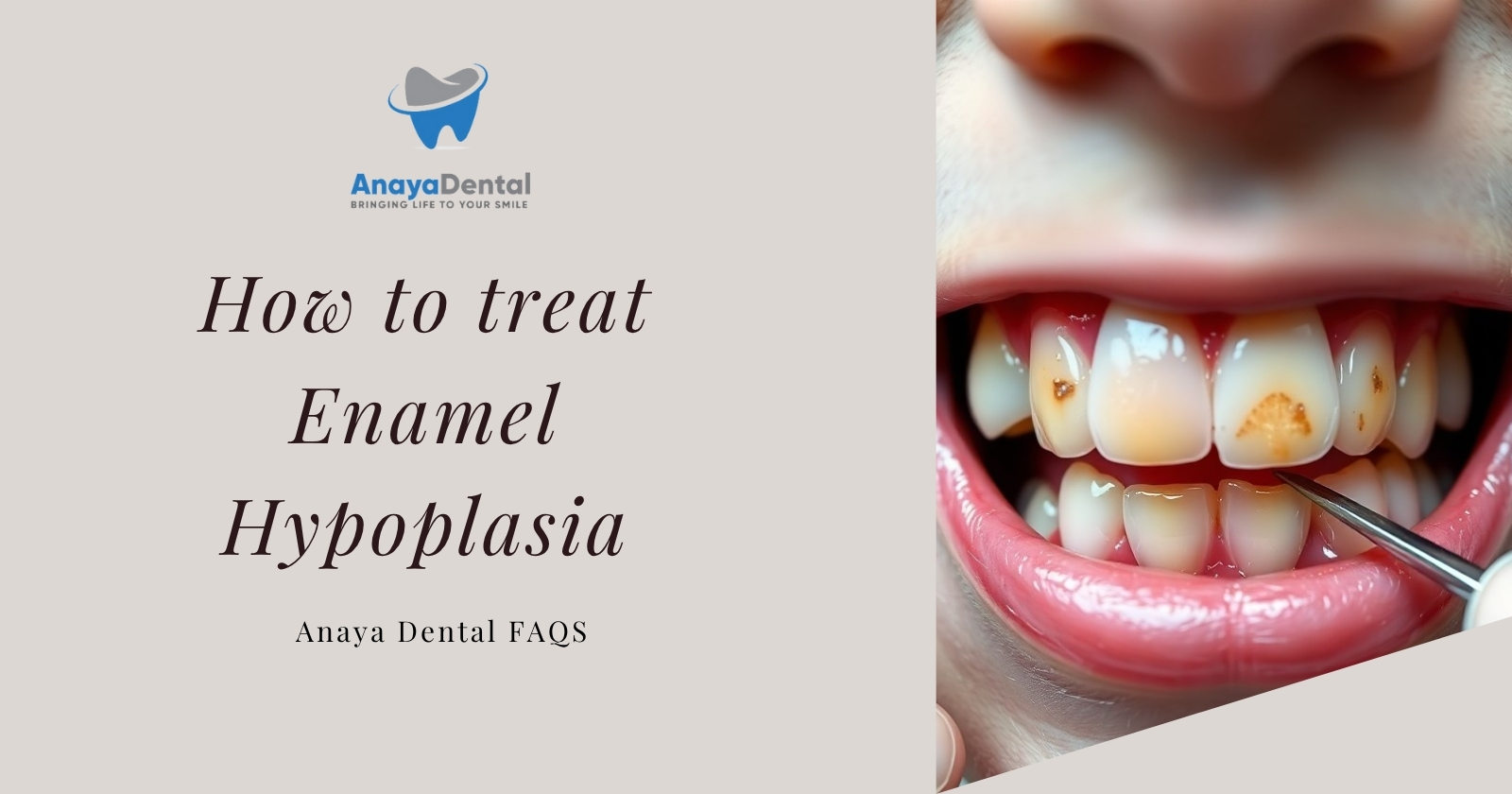
Treatment Options for Managing Enamel Hypoplasia
Conservative Approaches for Mild Cases
If your enamel hypoplasia is mild, your dentist might recommend conservative treatments:
- Professional fluoride treatments using high-concentration varnishes or gels to strengthen remaining enamel and reduce sensitivity
- Remineralization therapies with calcium phosphate products to enhance mineral content in affected areas
- Dental sealants applied to pitted areas to prevent decay and protect vulnerable spots
- Sensitivity management using specialized toothpastes and in-office desensitizing treatments
These approaches focus on preserving your natural tooth structure while improving function and comfort.
Restorative Options for Moderate to Severe Hypoplasia
For more pronounced defects, restorative treatments may be necessary:
- Dental bonding using tooth-colored composite resin can effectively mask defects while providing some structural support to weakened areas. This relatively affordable option works well for front teeth with moderate hypoplasia.
- Porcelain veneers offer a more durable and aesthetically pleasing solution for visible teeth with significant defects. These thin ceramic shells cover the front surface of teeth, completely masking hypoplastic areas while providing excellent color stability.
- Dental crowns may be recommended when defects are extensive or affect the structural integrity of your teeth. Full-coverage crowns protect the entire tooth and restore both appearance and function, though they require more tooth reduction than other options.
The appropriate restorative approach depends on defect severity, location, your age, expectations, and budget constraints.
Comprehensive Treatment Planning for Complex Cases
If you have severe enamel hypoplasia affecting multiple teeth, your dentist might develop a comprehensive treatment plan that:
- Addresses immediate concerns like sensitivity and decay risk
- Provides interim solutions while you’re still growing (if you’re young)
- Establishes a long-term restoration strategy that may unfold over several years
- Considers orthodontic needs alongside restorative treatments
- Incorporates preventive measures to protect unaffected teeth
Complex cases often benefit from a multidisciplinary approach involving pediatric dentists, orthodontists, and restorative specialists working together to achieve optimal outcomes.
Living With and Managing Enamel Hypoplasia Day to Day
Specialized Oral Hygiene Practices for Affected Teeth
If you have enamel hypoplasia, your daily oral care routine requires special attention:
- Use a soft-bristled toothbrush and gentle technique to avoid damaging vulnerable areas
- Consider electric toothbrushes with pressure sensors to prevent excessive force
- Apply high-fluoride toothpaste (prescribed by your dentist) to strengthen remaining enamel
- Use remineralizing products containing calcium phosphate compounds daily
- Clean between teeth carefully, especially around hypoplastic areas prone to plaque retention
- Consider fluoride mouth rinses for additional protection against decay
These specialized practices help maintain the integrity of your compromised enamel and reduce the risk of complications.
Dietary Considerations to Protect Weakened Enamel
Your diet plays a significant role in managing enamel hypoplasia:
- Limit consumption of acidic foods and beverages (citrus, sodas, sports drinks) that can further erode vulnerable enamel
- Reduce intake of sugary foods and drinks that fuel acid-producing bacteria
- Consume calcium-rich foods (dairy products, leafy greens, fortified alternatives) to support remineralization
- Include phosphorus sources (lean meats, eggs, nuts) to provide essential minerals for enamel
- Ensure adequate vitamin D through sun exposure, diet, or supplements to enhance calcium utilization
- Consider using a straw when drinking potentially harmful beverages to minimize contact with affected teeth
These dietary adjustments help protect your compromised enamel from further damage while providing nutrients that support oral health.
Managing Aesthetic Concerns and Building Confidence
The visible nature of enamel hypoplasia can sometimes affect your self-confidence, particularly if front teeth are involved. Consider these approaches:
- Discuss cosmetic concerns openly with your dental professional, who can suggest appropriate solutions based on your specific situation
- Explore temporary options like composite bonding if you’re not ready for permanent treatment
- Consider joining support groups or online communities where others share similar experiences
- Practice positive self-talk and remember that minor dental variations are completely normal
- Focus on maintaining excellent oral hygiene to keep your smile as healthy as possible regardless of appearance
Remember that modern dentistry offers multiple solutions for addressing the aesthetic aspects of enamel hypoplasia at various price points.
Preventive Strategies for Future Generations
Prenatal and Early Childhood Nutrition
Proper nutrition during pregnancy and early childhood plays a crucial role in preventing enamel hypoplasia:
- During pregnancy, expectant mothers should maintain adequate intake of calcium, phosphorus, and vitamin D to support the developing child’s tooth formation
- Infants and young children need balanced nutrition rich in essential minerals and vitamins
- Vitamin D supplementation may be recommended during pregnancy and early childhood, especially in regions with limited sun exposure
- Early identification and management of conditions affecting nutrient absorption, such as celiac disease, can help prevent nutritional deficiencies that might impact enamel formation
Research shows that maternal vitamin D levels significantly impact dental outcomes in children, with deficiencies increasing the risk of enamel hypoplasia and subsequent dental decay.
Monitoring and Managing Childhood Illnesses
Proper management of childhood illnesses can help reduce the risk of enamel hypoplasia:
- Prompt treatment of high fevers during early childhood
- Careful monitoring of medications prescribed during tooth development years
- Regular medical check-ups to identify and address nutritional deficiencies
- Special attention to oral health during and after serious childhood illnesses
- Awareness of the potential dental impacts of treatments for chronic conditions
Healthcare providers should consider the timing of tooth development when treating young children, particularly when prescribing medications that might affect enamel formation.
Early Dental Visits and Developmental Monitoring
Regular dental care from an early age allows for the monitoring of tooth development and early intervention:
- Schedule your child’s first dental visit by age one or when the first tooth erupts
- Maintain regular check-ups every six months to monitor dental development
- Report any unusual appearances in emerging teeth to your dental professional
- Follow preventive recommendations for fluoride use appropriate to your child’s age and risk factors
- Consider dental sealants for newly erupted permanent molars to provide additional protection
These preventive approaches can help identify and address potential issues before they progress to more severe problems requiring extensive treatment.
Emerging Research and Future Treatments
The field of dental research continues to advance our understanding of enamel hypoplasia and potential treatments:
- Biomimetic approaches aim to replicate natural enamel formation processes for better restoration options
- Stem cell research explores the possibility of regenerating dental tissues, including enamel
- Improved diagnostic tools help identify early signs of enamel defects before teeth even erupt
- Novel remineralization technologies show promise for enhancing the natural repair of minimally damaged enamel
- Genetic research provides insights into hereditary forms of enamel hypoplasia, potentially leading to targeted interventions
These developing technologies and approaches offer hope for even better management of enamel hypoplasia in the future.
Conclusion: Taking Control of Your Dental Health
Living with enamel hypoplasia presents unique challenges, but with proper understanding and care, you can maintain a healthy, functional smile. Early diagnosis, appropriate treatment, and consistent preventive measures are key to managing this condition effectively.
Remember that enamel hypoplasia, while not always preventable, is highly manageable with modern dental approaches. By working closely with your dental professional, you can develop a personalized care plan that addresses your specific concerns and helps preserve your dental health for years to come.
If you’ve noticed signs of enamel hypoplasia in your teeth or your child’s developing dentition, schedule a dental consultation to discuss your observations and explore appropriate treatment options. With proper care and attention, you can overcome the challenges of enamel hypoplasia and enjoy a healthy, confident smile.