If you’ve noticed a white coating on your tongue, you’re experiencing a common oral health condition. This white appearance occurs when the small bumps (papillae) on your tongue become inflamed and trap dead cells, bacteria, fungi, and food debris. While often harmless and temporary, a white-coated tongue can sometimes signal underlying health issues that require your attention.
Your tongue serves as a window into your overall health. Changes in its appearance often reflect changes in your body’s internal conditions, making it an important indicator for you and healthcare professionals to monitor. Understanding what causes your white tongue and how to treat it is essential not just for maintaining good oral health, but for your overall wellbeing.
What Causes Your White Tongue?
Poor Oral Hygiene
When you don’t clean your tongue regularly, a biofilm of bacteria accumulates on its surface. This biofilm consists of bacteria, fungi, food particles, and dead cells that adhere to your tongue’s surface, creating that visible white coating you see in the mirror.
Try Our Dental Calculators
Even if you brush your teeth twice daily, you can still develop white tongue if you neglect tongue cleaning. The textured surface of your tongue, with its many papillae, creates an ideal environment for bacterial colonization. These bacteria thrive in the warm, moist conditions of your mouth and multiply rapidly when not regularly removed through cleaning.
The back portion of your tongue is particularly susceptible to bacterial accumulation since it’s harder to reach when brushing.
Dehydration
When your body lacks adequate fluid, your saliva production decreases. Saliva plays a crucial role in your oral health by continuously washing away bacteria and food particles. When your saliva flow diminishes due to dehydration, these particles and bacteria remain on your tongue’s surface longer, contributing to white coating formation.
Signs that dehydration is causing your white tongue include dry mouth, increased thirst, darker urine, and dry skin. You may notice the white coating appears thicker in the morning after hours without fluid intake during sleep, and may temporarily improve after drinking water.
Even mild chronic dehydration can affect your tongue’s appearance, making adequate hydration essential for maintaining a healthy tongue.
Dry Mouth (Xerostomia)
If you suffer from dry mouth (xerostomia), you’re experiencing a specific reduction in saliva production that may result from various medical conditions or medications, rather than just inadequate fluid intake.

Medical causes that might be affecting your dry mouth include autoimmune conditions like Sjögren’s syndrome, diabetes, salivary gland disorders, and nerve damage affecting the salivary glands. If you’ve undergone radiation therapy for head and neck cancers, this can also damage your salivary glands, resulting in chronic dry mouth.
Several medications you might be taking list dry mouth as a side effect, including:
- Antihistamines
- Decongestants
- Antidepressants
- Antihypertensives
- Diuretics
- Anti-anxiety medications
- Pain medications
- Parkinson’s disease medications
- Muscle relaxants
Without adequate saliva, oral bacteria flourish in your mouth, leading to not just white tongue but also increased risk of tooth decay, gum disease, and oral infections.
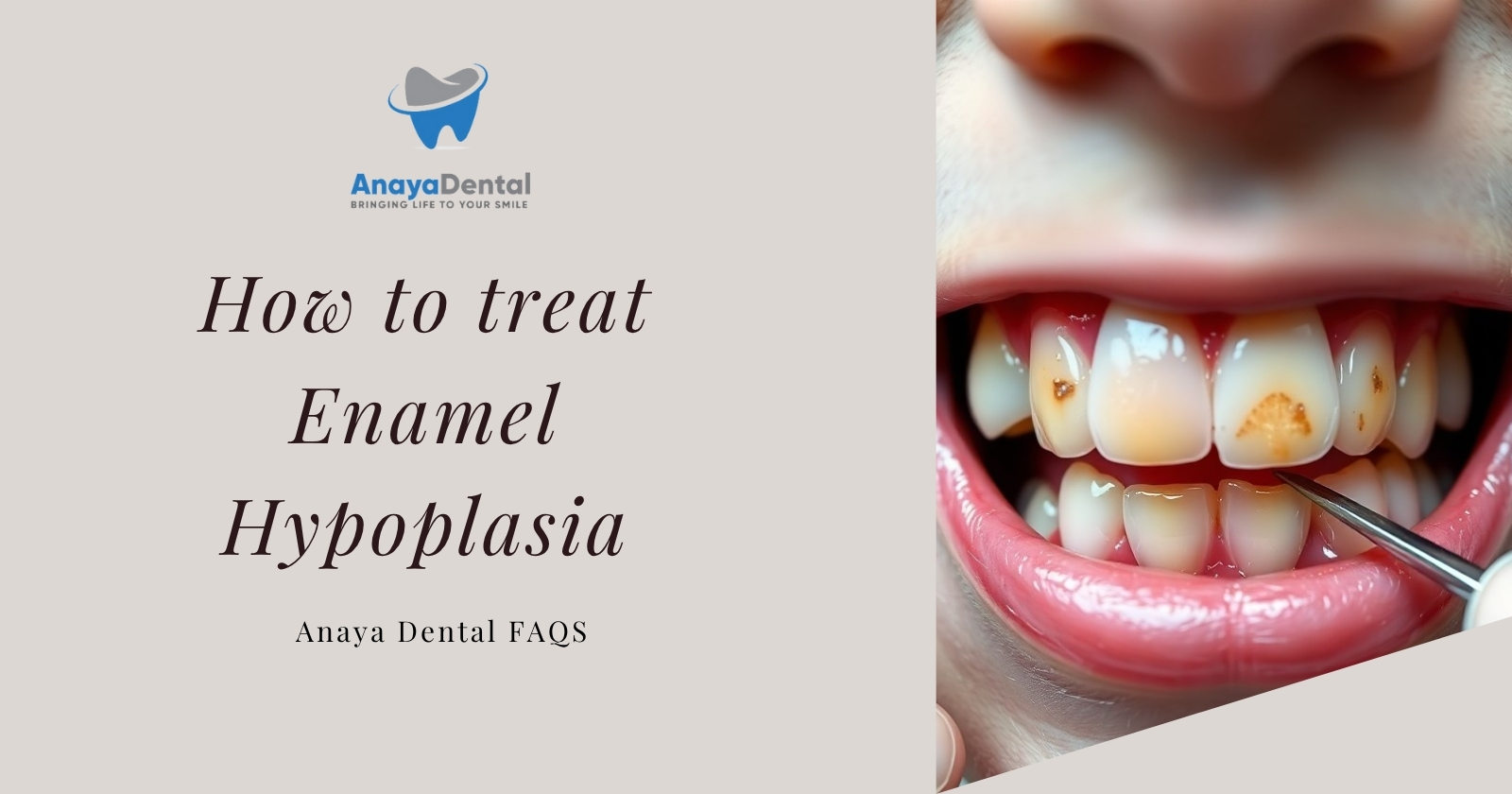
Oral Thrush (Candidiasis)
If you have oral thrush, you’re experiencing a fungal infection caused by an overgrowth of Candida albicans, a type of yeast naturally present in many people’s mouths. When certain conditions disrupt the normal balance of microorganisms in your mouth, Candida can multiply excessively, resulting in infection.

Unlike some other causes of white tongue, if you have thrush, you’ll typically notice creamy white, slightly raised lesions on your tongue, inner cheeks, and sometimes other oral surfaces. These lesions can be painful and may bleed slightly when scraped. A distinguishing characteristic of thrush is that the white patches cannot be easily scraped off, unlike food debris or other types of coating.
You may be at higher risk for developing oral thrush if you have:
- A weakened immune system (due to HIV/AIDS, cancer treatments, or certain medications)
- Diabetes (especially when poorly controlled)
- Recently used antibiotics
- Used corticosteroids (including inhaled corticosteroids for asthma)
- Dentures (especially if not properly cleaned)
- A smoking habit
- Very young or advanced age
Tobacco and Alcohol Use
If you use tobacco or consume alcohol regularly, you’re significantly impacting your oral health and contributing to white tongue formation through multiple mechanisms.
When you smoke or chew tobacco, you’re exposing your mouth to numerous chemicals that irritate your oral tissues, including your tongue. This irritation can cause inflammation of your papillae, creating more surface area for debris and bacteria to accumulate. Smoking also reduces your saliva production and impairs its quality, diminishing your mouth’s natural cleaning mechanism.
Your long-term tobacco use can lead to more serious conditions like leukoplakia (white patches that cannot be rubbed off) and hairy leukoplakia (fuzzy white patches, particularly on the sides of your tongue).
If you consume alcohol, especially heavily or frequently, you may experience dehydration and reduced saliva production. Alcoholic beverages—particularly those with high alcohol content—can irritate your oral mucosa, potentially leading to inflammation.
If you use both tobacco and alcohol, you’re creating a particularly high-risk scenario for oral health problems, including persistent white tongue and more serious conditions.
Dietary Factors Affecting Your Tongue
What you eat plays a significant role in your tongue health and appearance. Certain foods and beverages can directly contribute to your white tongue, while nutritional deficiencies can affect the health of your oral tissues.
Foods and beverages that may be contributing to your white tongue include:
- Soft, processed foods that don’t provide the mechanical cleaning action that fibrous foods offer
- Sugary foods and drinks that feed oral bacteria
- Dairy products, which can temporarily coat your tongue
- Coffee and tea, which can stain your tongue and contribute to dry mouth
- Spicy foods that may irritate your tongue surface
If your diet lacks certain nutrients, this may affect your tongue health:
- Iron deficiency can cause a pale tongue and reduced immunity to oral infections
- B vitamin deficiencies (particularly B12) can affect your tongue tissue health
- Zinc deficiency impacts taste and can affect your oral tissue integrity
- Folic acid deficiency can lead to inflammation of your tongue (glossitis)
If your diet is high in processed foods and low in fresh fruits and vegetables, you may not be getting adequate nutrients for optimal oral health.
Medical Conditions That May Be Causing Your White Tongue
Several specific medical conditions may be causing your white tongue:
Geographic tongue presents as irregular, smooth, red patches surrounded by white borders on your tongue’s surface. These patches may appear to migrate over time, giving your tongue a map-like appearance. While generally harmless, you may experience sensitivity or burning sensations, especially with spicy or acidic foods.

Leukoplakia appears as thick, white patches on your tongue that cannot be scraped off. Unlike thrush, your leukoplakia is not caused by a fungal infection but is often associated with chronic irritation, particularly from tobacco use. Some leukoplakia patches may become cancerous, making medical monitoring essential.
Oral lichen planus is an inflammatory condition that can affect the mucous membranes of your mouth. On your tongue, it may appear as white, lacy patches or lines. This chronic condition is thought to be autoimmune-related and may cause you discomfort or pain.
Syphilis, a sexually transmitted infection, can cause white patches on your tongue and mouth during its secondary stage. These patches, known as mucous patches, may be painless but are highly infectious.
Hairy leukoplakia presents as white, hairy patches that typically appear on the sides of your tongue. Unlike regular leukoplakia, hairy leukoplakia is caused by the Epstein-Barr virus and is particularly common if you have a weakened immune system, especially due to HIV/AIDS.
When You Should See a Doctor
While you can self-diagnose and treat many cases of white tongue at home, you should consider consulting a healthcare provider if:
- Your white tongue persists for more than two weeks despite improved oral hygiene
- The white coating is thick, doesn’t scrape off, or quickly returns after cleaning
- You experience pain, burning sensations, or difficulty swallowing or speaking
- You notice unusual changes in taste or breath
- You have open sores or bleeding from your tongue
- You have a weakened immune system due to conditions like diabetes, HIV/AIDS, or cancer treatments
- White patches appear alongside other concerning symptoms
During your examination, your healthcare provider will typically:
- Review your medical history, including medications, existing health conditions, tobacco and alcohol use, and oral hygiene practices
- Conduct a physical examination of your mouth, including your tongue, cheeks, gums, and palate
- Assess the appearance, texture, and distribution of the white coating or patches
- Check for other oral health issues that might be related
- Consider your overall health status and symptoms
Your doctor might perform diagnostic tests including:
- Scraping a sample for microscopic examination or culture
- Biopsy for suspicious lesions
- Blood tests to check for underlying conditions
- Saliva flow rate measurements if dry mouth is suspected
How You Can Treat White Tongue
At-Home Remedies You Can Try
Proper tongue cleaning techniques form the foundation of treating your white tongue:
- Use a tongue scraper designed for this purpose rather than your toothbrush when possible
- Start at the back of your tongue and gently pull forward, rinsing the scraper between strokes
- Apply gentle pressure—enough to remove coating but not so much that it causes pain or bleeding
- Clean your tongue once or twice daily, ideally after brushing your teeth
- Be thorough but gentle with the back of your tongue where gag reflexes may be triggered
The best tools for cleaning your tongue include:
- Tongue scrapers made of copper, stainless steel, or plastic (copper has additional antimicrobial properties)
- Soft-bristled toothbrushes if scrapers aren’t available
- Specialized tongue brushes with shorter bristles designed specifically for tongue cleaning
To combat white tongue through proper hydration:
- Drink at least 8-10 glasses of water daily
- Limit dehydrating beverages like alcohol and caffeine
- Use alcohol-free mouthwash to avoid further mouth dryness
- Breathe through your nose rather than mouth when possible
- Use a humidifier if you live in a dry climate or during winter months
You can try salt water rinses to help reduce bacterial load and inflammation. Mix 1/2 teaspoon of salt in a cup of warm water and rinse your mouth for 30 seconds, 2-3 times daily.
Baking soda solutions can help neutralize acids and reduce bacteria. Mix 1/2 teaspoon of baking soda in a cup of warm water for rinsing, or make a paste with a few drops of water for gentle scrubbing.
Oil pulling—swishing a tablespoon of coconut or sesame oil in your mouth for 10-15 minutes before spitting it out—has some anecdotal support and may help bind to bacteria in your mouth.
Lifestyle Changes That Will Help
Several lifestyle modifications can improve your white tongue condition:
Quit tobacco in all forms. This is perhaps the most impactful change if you use tobacco products. Tobacco cessation not only helps resolve your white tongue but prevents more serious oral conditions, including cancer.
Reduce alcohol consumption to maintain proper hydration and saliva production. Limiting your intake to moderate levels or abstaining completely can significantly improve your oral health.
Modify your diet by:
- Increasing consumption of fibrous fruits and vegetables that naturally clean your tongue
- Reducing sugar intake to limit bacterial growth
- Ensuring adequate intake of nutrients important for oral health, particularly B vitamins, iron, and zinc
- Adding probiotic foods like yogurt to promote a healthy oral microbiome
- Staying well-hydrated throughout the day
Improve your general oral hygiene by:
- Brushing teeth thoroughly twice daily
- Flossing daily to remove interdental plaque
- Using an antiseptic mouthwash
- Replacing your toothbrush every 3-4 months
- Attending regular dental check-ups
Medical Treatments You Might Need
When home remedies and lifestyle changes aren’t enough to resolve your white tongue, you might need medical interventions:
Antifungal medications may be prescribed if you have oral thrush. These may include:
- Nystatin oral suspension or lozenges
- Clotrimazole lozenges
- Fluconazole tablets for more severe or resistant cases
Your doctor may treat underlying conditions depending on your specific diagnosis:
- Medications to stimulate your saliva production for chronic dry mouth
- Immune system support if you have conditions like HIV/AIDS
- Nutritional supplements if you have deficiencies
- Antibiotics if you have a bacterial infection
How to Prevent White Tongue
Your Daily Oral Care Routine
To prevent white tongue, implement this optimal oral hygiene routine:
- Brush your teeth at least twice daily for two minutes using fluoride toothpaste
- Floss once daily to remove interdental plaque
- Clean your tongue once or twice daily
- Use an antimicrobial or alcohol-free mouthwash once daily
- Replace your toothbrush every 3-4 months or sooner if bristles are frayed
For specific tongue care:
- Use a tongue scraper rather than a toothbrush when possible
- Clean your entire tongue surface, including the back (where most bacteria reside)
- Use gentle pressure to avoid damaging tongue tissue
- Clean your tongue scraper thoroughly after each use
- Replace tongue scrapers regularly to prevent bacterial buildup
Your Hydration and Diet
To maintain optimal oral hydration:
- Drink at least 8-10 glasses of water daily
- Increase your intake during hot weather, exercise, or illness
- Limit your alcohol and caffeine consumption
- Consume hydrating foods like fruits and vegetables
- Consider using sugar-free lozenges or gum to stimulate saliva if your mouth tends to be dry
A diet that supports your tongue health includes:
- Adequate protein for tissue maintenance and repair
- Sufficient B vitamins, particularly B12, B9 (folate), and B2 (riboflavin)
- Iron-rich foods to prevent anemia-related tongue changes
- Zinc-containing foods for taste function and tissue integrity
- Vitamin C for gum health and immune function
- Antioxidant-rich foods to fight inflammation
- Probiotic foods to support a healthy oral microbiome
- Limited refined sugars and processed foods
When You Should Expect Improvement
Timeline for Recovery
| Cause of White Tongue | When You’ll Notice Improvement | Time for Complete Resolution |
|---|---|---|
| Poor oral hygiene | 2-3 days with proper cleaning | 1-2 weeks with consistent care |
| Dehydration | Hours to days with proper hydration | 1-4 days with maintained hydration |
| Oral thrush | 48-72 hours after starting antifungals | 7-14 days with full treatment course |
| Medication-induced | 1-2 weeks after addressing cause | Varies based on medication changes |
| Tobacco-related | 1-2 weeks after cessation | Up to several months for heavy users |
| Dry mouth conditions | Varies with treatment | May require ongoing management |
| Underlying medical conditions | Depends on successful treatment | May be chronic depending on condition |
For white tongue caused by poor oral hygiene, dehydration, or minor irritation, you’ll often notice improvement within days of implementing proper tongue cleaning and hydration. You can expect complete resolution typically within 1-2 weeks with consistent care.
If you have oral thrush, you’ll usually notice improvement within 48-72 hours of beginning antifungal treatment, with complete resolution typically occurring within 7-14 days.
If your white tongue is associated with underlying medical conditions, your timeline depends on the effectiveness of treating those conditions and may take longer to resolve completely.
When You Should Worry About Recurrence
You should seek further investigation if your white tongue:
- Returns quickly after successful treatment
- Becomes progressively worse with each episode
- Develops alongside new symptoms
- Begins affecting your eating, speaking, or quality of life
- Appears alongside unexplained symptoms elsewhere in your body
Special Considerations for Your Situation
If You’re Pregnant
If you’re pregnant, you may experience changes in oral health due to hormonal fluctuations, dietary changes, and sometimes altered oral hygiene routines.
Your white tongue during pregnancy may result from:
- Hormonal changes affecting your oral microbiome
- Morning sickness and vomiting altering your oral pH
- Food cravings leading to increased sugar consumption
- Heightened gag reflexes making tongue cleaning more difficult
- Immune system changes making fungal infections like thrush more likely
- Pregnancy-related fatigue impacting your oral care routines
Safe treatment options during your pregnancy:
- Standard oral hygiene practices including tongue cleaning are safe and recommended
- Salt water rinses are safe during pregnancy
- Natural remedies like yogurt consumption may help restore microbial balance
- Consult your healthcare provider before using any medications, including over-the-counter products
If You’re a Senior
As you age, you face several factors that increase your risk of white tongue:
- Decreased saliva production as a natural part of aging
- Reduced immune function
- Changes in nutritional status and eating patterns
- Reduced manual dexterity for oral hygiene tasks
- More frequent mouth breathing, especially during sleep
- Higher rates of denture use, which can harbor fungi and bacteria
Many medications commonly prescribed to older adults cause dry mouth, and taking multiple medications can compound these effects.
To adapt your treatment:
- Consider electric toothbrushes and specialized tongue cleaning tools to help overcome dexterity issues
- Ask your doctor about saliva substitutes for chronic dry mouth
- If you wear dentures, implement specific cleaning routines for both dentures and oral tissues
- Ask for assistance with oral care if you have physical limitations
For Your Child
If your child has white tongue, consider these common causes specific to children:
- Oral thrush, which is particularly common in infants due to their developing immune systems
- Dehydration from inadequate fluid intake or illness with fever
- Poor oral hygiene as children learn proper brushing habits
- Mouth breathing, common in children with allergies or enlarged adenoids
To treat your child’s white tongue:
- For infants with thrush, your pediatrician may prescribe antifungal drops or gel
- For older children, make tongue cleaning fun and part of a routine to improve compliance
- Consider child-friendly tongue scrapers with appealing designs
- Use flavored (but sugar-free) mouth rinses to encourage use
- Implement rewards systems for consistent oral hygiene to help establish lifelong habits
You should be attentive to white tongue in your child, especially if it persists beyond a few days or is accompanied by refusal to eat, drooling, fever, or irritability.
Frequently Asked Questions About Your White Tongue
Is your white tongue contagious?
Most causes of your white tongue are not contagious. However, if you have oral thrush (candidiasis), it can potentially spread through direct contact, particularly through kissing or sharing eating utensils. This is more likely if one person has a weakened immune system.
Non-infectious causes of your white tongue—such as those related to poor oral hygiene, dehydration, tobacco use, or medication side effects—cannot be transmitted to others.
Does your white tongue affect your taste?
Yes, your white tongue can affect your taste perception in several ways:
- The physical coating creates a barrier between your taste buds and food, dulling taste sensations
- Underlying conditions causing your white tongue, particularly fungal infections, can directly affect your taste bud function
- Dry mouth, which often accompanies white tongue, reduces the dissolution and delivery of flavor molecules to your taste receptors
- The bad breath that sometimes accompanies your white tongue can impact how you perceive flavors since taste and smell are closely linked
Your taste changes will typically resolve when your white tongue condition is effectively treated.
Can stress cause your white tongue?
Yes, stress can indirectly contribute to your white tongue through several mechanisms:
- Stress hormones can suppress your immune function, potentially allowing for overgrowth of fungal or bacterial organisms
- Your stress often disrupts sleep, which can impact immune function
- During stress, you may neglect your oral hygiene routines
- Your stress may lead to dehydration if your fluid intake decreases
- Stress-related habits like increased smoking, alcohol consumption, or poor dietary choices can affect your oral health
- You may breathe more through your mouth when anxious, leading to dry mouth
While stress alone is rarely the sole cause of your white tongue, managing your stress through techniques like meditation, adequate sleep, regular exercise, and sometimes professional support can be an important component of your treatment.
Are probiotics helpful for your white tongue?
The oral microbiome—the community of microorganisms in your mouth—plays a significant role in your tongue health. When this microbial balance is disrupted, opportunistic bacteria or fungi can overgrow, potentially contributing to your white tongue.
Probiotics may help restore this balance in your mouth through several mechanisms:
- Competing with harmful microorganisms for nutrients and attachment sites
- Producing antimicrobial substances that inhibit pathogen growth
- Modulating your local immune responses to better control microbial populations
- Reducing inflammation that contributes to papillae inflammation
Research specifically examining probiotics for white tongue is limited, but studies on oral thrush prevention show promising results, particularly for Lactobacillus-containing probiotics. Probiotic lozenges or rinses applied directly in your mouth appear more effective than systemic supplementation for oral conditions.
While not a standalone treatment, including probiotic foods (like unsweetened yogurt) or supplements may be a helpful addition to your conventional white tongue treatments.
How can you tell if your white tongue indicates something serious?
While most cases of white tongue are benign, you should be concerned if your white tongue has these warning signs:
- White patches that persist in the same location for weeks
- Patches with red components (erythroleukoplakia)
- Patches that cannot be scraped off
- Hardened or rough texture of the patches
- Unexplained bleeding or ulceration
- Pain or numbness in the affected area
You should seek medical evaluation if:
- Your white patches cannot be scraped off
- Your white tongue lasts more than two weeks despite improved oral hygiene
- You experience pain, burning, or tenderness of your tongue
- You have difficulty swallowing, speaking, or moving your tongue
- You have open sores or ulcers on your tongue
- You notice unusual bleeding from your tongue or mouth
Be particularly vigilant about seeking care if your white tongue appears alongside:
- Unexplained weight loss
- Persistent fatigue
- Swollen lymph nodes in your neck
- Night sweats
- Fever without other explanation
- Difficulty breathing
- Rashes elsewhere on your body
Conclusion
Your white tongue, while often harmless, serves as an important indicator of your oral and sometimes overall health. By understanding its causes and implementing the right treatments, you can resolve this condition and maintain a healthier mouth.
Remember that most cases of white tongue respond well to improved oral hygiene, proper hydration, and lifestyle adjustments. However, if your symptoms persist or are accompanied by concerning signs, don’t hesitate to seek professional medical advice.
By incorporating regular tongue cleaning into your daily oral hygiene routine, staying well-hydrated, and addressing underlying factors like tobacco use or medication side effects, you can prevent recurrence and enjoy better oral health.