Dry socket has” troubled dentists ever since the practice of exodontia began”. It is one of the most perplexing post extraction complications. WHAT IS DRY SOCKET ?
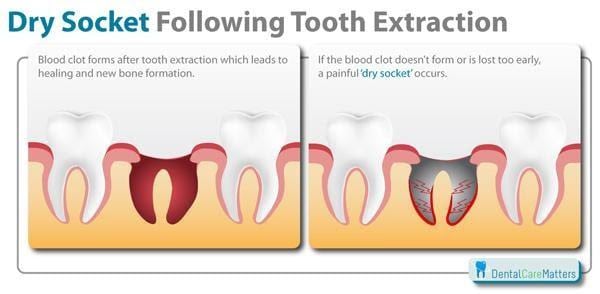
It is a term generally used to refer to delayed onset acute pain in an empty socket area due to loss of blood clot.
Contents
How common is dry socket?
Around 2- 4% of the population after removal of wisdom tooth develops dry socket. In normal conditions, there are very less chances of developing dry socket but there can be various complications/ causes that can lead to dry socket.
Now the question arises what are the causes of dry socket???…Though the causes are numerous and still under research the loss/ dislodgement of blood clot leading to dry socket is most common.
The onus of dry socket mainly lies on the patient in failure to comply with post extraction instructions. Vigorous mouth rinses, taking aerated beverages, smoking, continuous spitting, etc. are some of the most common reasons for loss of blood clot. Breakdown of clot exposes the bone and makes the socket area empty leading to bacterial infection.
What does a dry socket look like/how to diagnose dry socket
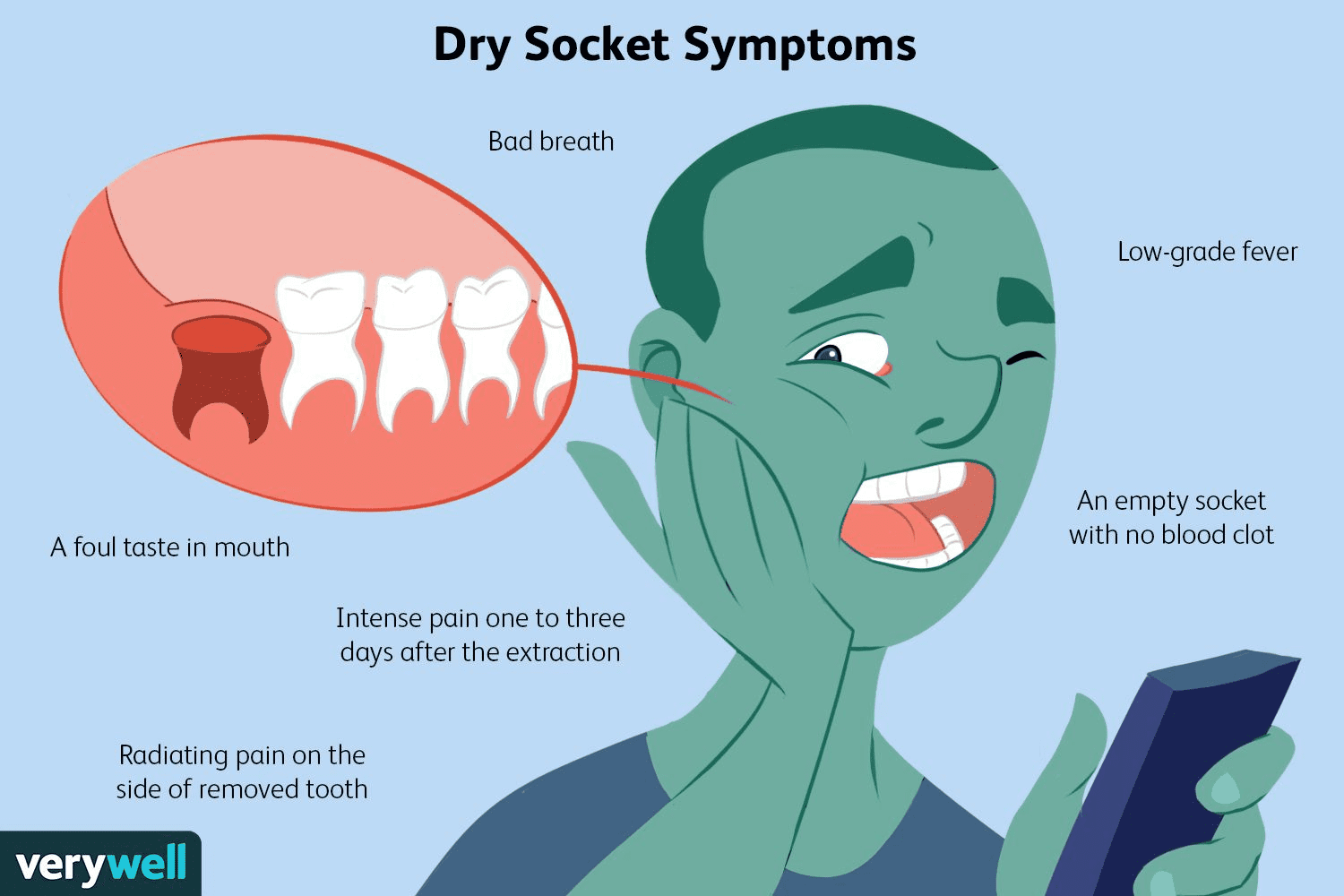
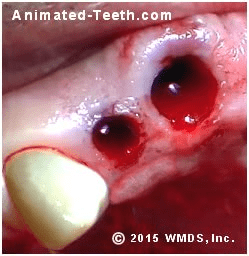
Dry socket doesn’t exhibit any fever, redness, edema or any pus formation in the socket area rather characterized by fetid odor and bad taste. A dry socket usually appears like a hole left after the tooth extraction. Around this hole perimeter exposed bone is visible. The space from which the tooth is extracted will appear empty and whitish in color.
After the tooth extraction blood clot is formed over the extraction site. This blood clot can be dislodged because of various reasons and then the bone, nerve endings get exposed. It is very important that the blood clot remains intact. Dislodged clot can cause the entrapment of food debris and further lead to decay by bacterias.
Pain usually starts by 3-5th day after extraction and can radiate to other areas. Pain becomes dull after some days due to necrosis of tissue in the socket. It can be diagnosed simply by passing a probe in the socket area, bare bone is felt which is extremely sensitive and painful.
What factors lead to dry socket
There are many predisposing factors for dry socket some of them are:-
Difficulty in extraction-
Vigorous bone removal and inept force application can lead to loss of blood supply to bone thereby causing devitalization of bone and prone to infection.
Is dry socket more common in mandible-
Dry socket is more common in mandible as bone is quite dense and less vascular as compared to upper jaw . Gravity also plays a major factor as food tends to get accumulated in the lower jaw area promoting bacterial growth and infection.
Radiation therapy
radiation therapy leads to decreased vascularity of bone thereby healing is delayed. It also increases chances of dry socket
Does taking oral contraceptives cause dry socket??
Oral contraceptives increase blood clot dissolution activity hence significantly increasing chances for dry socket.
SYMPTOMS OF DRY SOCKET
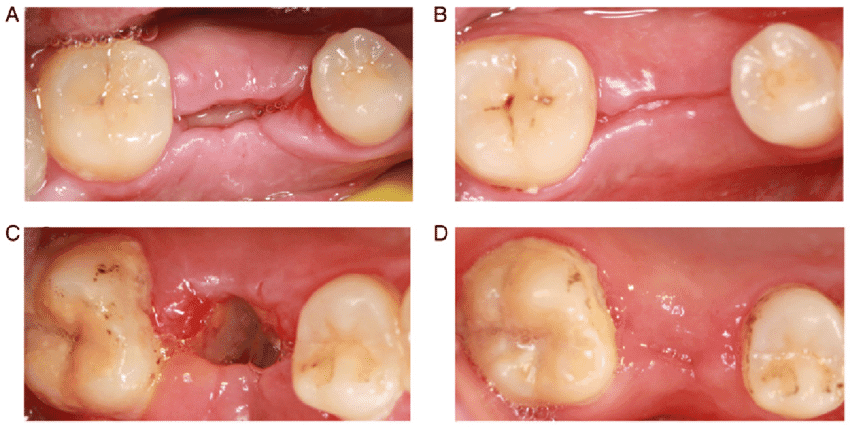
WHAT SHOULD A TOOTH EXTRACTION LOOK LIKE WHEN HEALING PICTURES
After the tooth extraction the empty socket heals on its own and the pain also subsides gradually. Blood clot is present over the extraction site. No bone is visible like a dry socket. Also, there is no foul breath or change in taste.
WHAT DOES BLOOD CLOT AFTER TOOTH EXTRACTION LOOK LIKE?
Immediately after the tooth extraction, the natural healing process will start. It is the same process as any other part of our body.
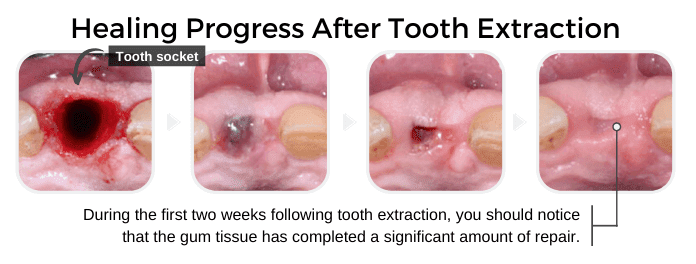
After 3- 4 minutes of extraction blood clot starts forming, to achieve stability and fixation of the clot in the socket area you should bite firmly over the gauze piece placed in the extraction area for about 45- 50 minutes. After removal of gauze you can see a gelatinous dark red clot formed in the socket area.
How to fix dry socket
Treatment aims at pain relief and promoting healing of the extraction area.
IF REPORTING WITHIN 48 HOURS:
The necrotic/dead blood clot is removed and fresh bleeding is induced under local anesthesia. Pressure pack is given with an antibiotic cover.
IF REPORTING AFTER 48 HOURS
In cases reported After 48 hours necrotic debris are removed with saline and the area is irrigated with betadine solution. After the irrigation area is packed with ribbon gauze soaked with zinc oxide eugenol paste to completely isolate the socket area from the oral cavity.
Pack should not be forcefully pushed into socket, it should gently cover the base of the socket.it protects the bare bone from food debris and other irritants. Eugenol acts as an obtundant and relieves pain.
Now, we will discuss a very common question amongst the population: “Will dry socket heal on its own?”
No, absolutely not. Bacterial accumulation and the infection in the socket area can cause prolonged pain referring to the ear and other parts of the jaw. Hence, apt intervention by your dentist is a must for better management and avoiding worrisome circumstances. Your dentist will thoroughly clean the infected socket area by flushing out all food debris and bacterial toxins and pack the socket with obtundant dressing. A short course of antibiotics along with painkillers is also advised.
Can you get dry socket with stitches?
Yes, though chances are less but you can have dry socket even after stitches. Stitches are to approximate the tissue borders to each other to help in healing but if you use straw or do smoking or can be another contributing factor then the healing process gets hampered and you can have the dry socket problem.




